How to Properly Read an EKG: Essential Guide for Current Medical Professionals in 2025
Understanding how to read an EKG is crucial for healthcare professionals, especially as advancements in medical technology continue to evolve. This guide provides a comprehensive overview of EKG interpretation, aiming to enhance your knowledge on EKG basics, waveforms, intervals, segments, and troubleshooting. Whether you are familiar with EKGs or looking to brush up on your skills, this article is packed with essential information for your practice.
1. EKG Basics: Fundamentals of EKG Interpretation
In order to effectively perform reading EKGs, you must start with the fundamentals. First, you should familiarize yourself with the EKG waves, which include the P wave, QRS complex, and T wave. Understanding these components is crucial for assessing the normal EKG compared to an abnormal EKG. Each waveform represents a specific phase of the cardiac cycle, indicating how the heart functions throughout its rhythm and rate.
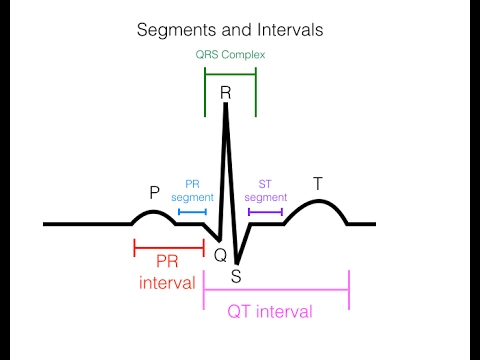
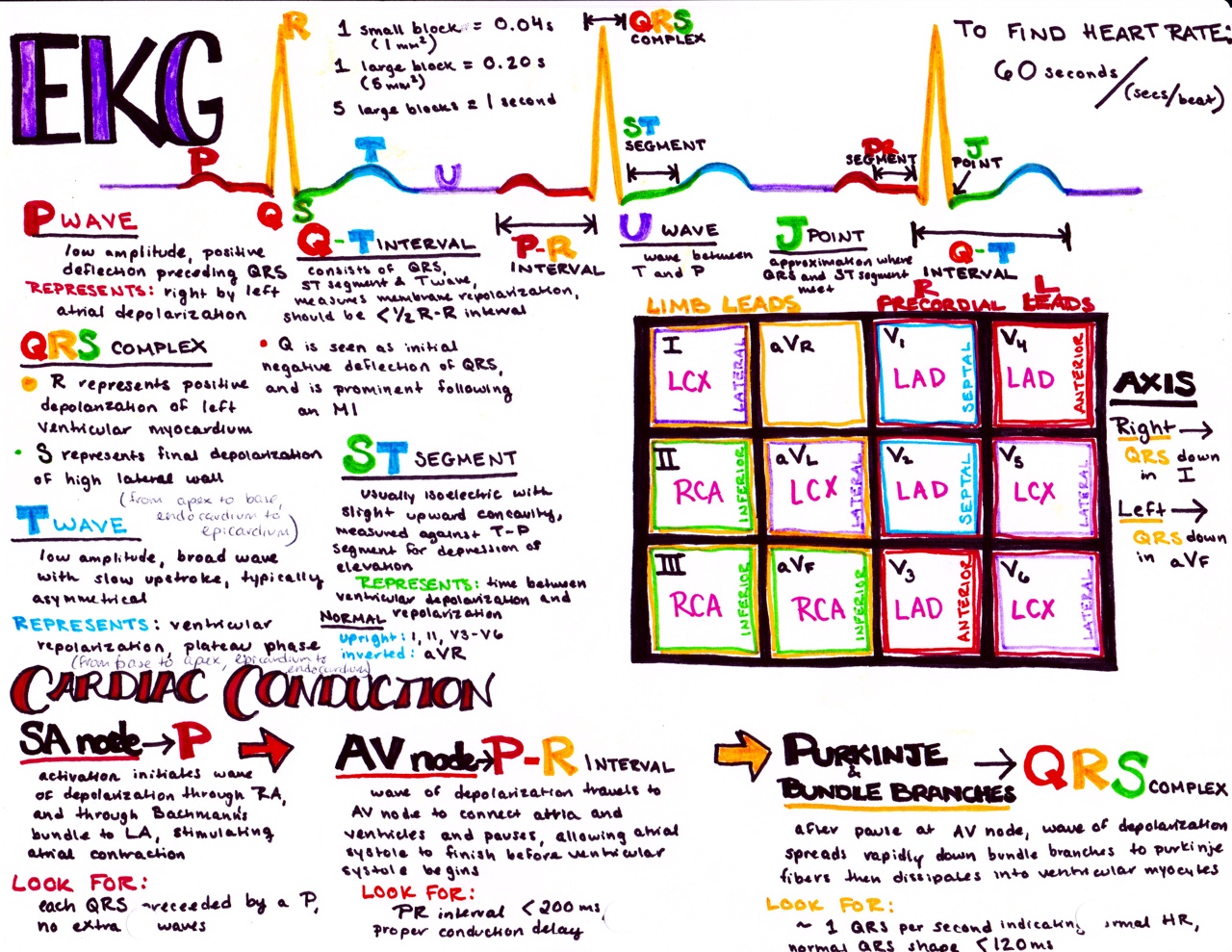
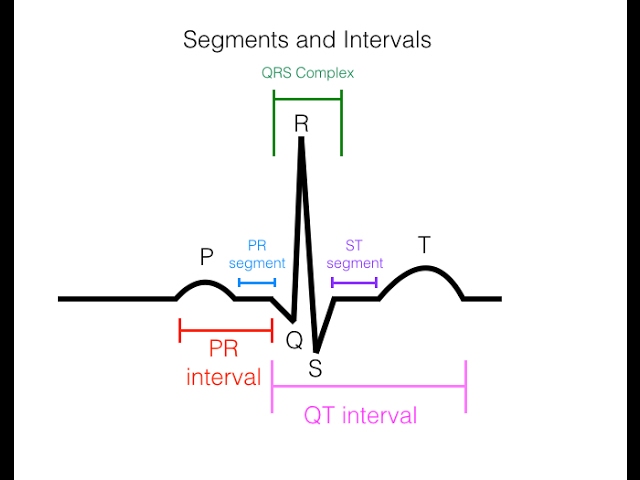
1.1 Understanding EKG Waves and Segments
The P wave indicates atrial depolarization, while the QRS complex signifies ventricular depolarization and is crucial for understanding EKG rhythms. The T wave reveals ventricular repolarization. Further breaking down segments, the PR interval reflects the time it takes for electrical impulses to move from the atria to the ventricles, while the ST segment can hint at conditions such as ischemia. Properly assessing these waves leads to better EKG analysis, improving diagnostic capabilities for conditions like myocardial infarction and atrial fibrillation.
1.2 EKG Intervals and Measurements
An essential skill in EKG analysis is measuring the EKG intervals. The QT interval, for example, is important for evaluating the risk of arrhythmias. Proper calibration of your EKG devices guarantees accurate readings, allowing the clinician to measure while also understanding how heart rates can vary significantly under different conditions, such as during stress tests. Standardized measurements help prevent issues related to EKG documentation and improve patient outcomes.
2. EKG Lead Placement: Ensuring Accurate Results
Precise EKG lead placement is vital to obtaining valuable data. Correctly positioning leads significantly affects the outcome and interpretation of trends and findings. It’s essential to use established guidelines for EKG monitoring to ensure you obtain clear and interpretable readings for effective clinical use.
2.1 Lead Configuration
In typical 12-lead EKG interpretation, hospital staff should ensure a standardized approach to lead placement. The six limb leads and six chest leads have specific anatomical placements and responsibilities. For instance, the classic camera technique requires ensuring the right arm lead is placed on the wrist while light skin cleaning agents might be applied. A visual representation can bolster understanding: learning through EKG viewing and visualization resources can boost clinician confidence.
2.2 Troubleshooting EKG Leads
Occasionally, EKG troubleshooting can become necessary to address artifacts or noise on the EKG. If a patient’s arms move or they experience jitter, it can compromise the quality of your readings. Knowledge of lead placement and a systematic troubleshooting guide are invaluable for accurate assessments and effective patient monitoring. Stick with standardized checks to ensure minimal errors are present during monitoring sessions, improving overall patient assessment.
3. Advanced EKG Techniques: Diagnostic and Clinical Strategies
By leveraging advanced EKG techniques, clinicians can take their EKG evaluation skills to new heights. For healthcare professionals in cardiology, understanding the nuances of identifying EKG abnormalities and employing technology effectively leads to superior outcomes.
3.1 Identifying EKG Patterns
Mastering the art of identifying EKG patterns is an essential skill that relies not only on experience but also on rigorous practice and education. Resources available through comprehensive EKG training and courses are beneficial, allowing professionals to build or enhance their capabilities in evaluating common cardiac rhythms and variations such as ventricular tachycardia and heart blocks.
3.2 EKG Evaluation Tools
The role of EKG software has never been more significant. Automate the analytical process with innovative technologies that assess patient data accurately. Tools can even analyze beats for distinct arrhythmias, rendering routine evaluations much more streamlined while helping clinicians focus on actionable findings. Updates in software often reach peak efficacy in settings that require rapid patient evaluations, helping teams manage simultaneous workloads effectively.
4. EKG Education and Resources for Health Professionals
The path to mastering how to read an EKG effectively is about continuous education and practice. Whether you are in a hospital, private office, or working in clinical settings, understanding advanced concepts and available learning materials is exhaustive. Engage with courses designed to further enhance your EKG education and build your confidence for patient assessment.
4.1 EKG Learning Resources
Explore EKG education materials by utilizing wide-ranging resources, such as webinars, online courses, books, and case studies. Emphasize finding materials suited for your particular context, whether it’s for beginners or ongoing advanced practice. These tailored resources can include practical simulations or specific clinical applications associated with reading EKG.
4.2 Community Workshops and Courses
Participate in community EKG workshops that delve into interpreting challenges. Engage with professionals in a collaborative environment that promotes shared learning. These interactions often prove invaluable in developing real-world diagnostic skills and precise analyses. Curriculum-based courses that emphasize EKG clinical correlations target both nursing and medical tracks effectively with real-life scenarios.
Key Takeaways
- Understanding how to read an EKG begins with familiarization with waveforms and intervals.
- Practicing EKG lead placement ensures accurate data capture for effective patient monitoring.
- Advanced EKG techniques are vital for correctly identifying rhythm abnormalities.
- Continuous EKG education through resources and community workshops enhances clinical skills!
FAQ
1. What is the significance of PQRST complex in EKG interpretation?
The PQRST complex illustrates the heart’s electrical activity during a heartbeat. Each component represents depolarization and repolarization of the heart chambers. Understanding this complex is crucial for identifying various pathologies such as ischemia or arrhythmias.
2. How do I troubleshoot frequent EKG artifacts?
Frequent EKG artifacts may indicate poor lead placement or patient movement. Ensuring proper attachment of leads and instructing patients to remain still can dramatically reduce issues. Always revisit clean lead techniques as well.
3. Why is EKG training essential for professionals?
Effective EKG training underpins accurate diagnosis and treatment plans. A poor understanding of ECG could lead to misinterpretation and patient risk. Continuous education solidifies one’s abilities and confidence when working through complex cases.
4. What are the recommended guidelines for EKG lead placement?
Standard guidelines involve placing leads directly to specified anatomical locations. Follow AHA or ACC recommendations, ensuring consistency across all EKG recordings to eliminate variation and improve diagnostic accuracy.
5. Is EKG evaluation solely for cardiological care?
No, while essential in cardiology, EKGs serve various medical contexts, including emergency medicine, patient monitoring, and even interpretative exercises for new physicians and interns.